CANCER TREATMENTS – TACE, RFA, EMBOLIZATION
Cancer Treatments – TACE, RFA, Embolization
Trans arterial chemoembolization is a minimally invasive procedure performed in interventional radiology to restrict a tumor’s blood supply. Small embolic particles coated with chemotherapeutic drugs are injected selectively through a catheter into an artery directly supplying the tumor. These particles both block the blood supply and induce cytotoxicity, attacking the tumor in several ways.

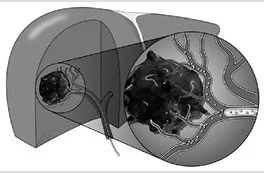

Transcatheter arterial chemoembolization has most widely been applied to Hepatocellular carcinoma of liver for patients who are not eligible for surgery. TACE has been shown to increase survival in patients with intermediate HCC by BCLC criteria. It has also been used as an alternative to surgery for resectable early stage HCC and in patients with regional recurrence of the tumor after previous resection. TACE may also be used to downstage HCC in patients who exceed the Milan criteria for liver transplantation.
Other treated malignancies include neuroendocrine tumors, ocular melanoma, cholangiocarcinoma, and sarcoma. Transcatheter arterial chemoembolization plays a palliative role in patients with metastatic colon carcinoma. There is a possible benefit for liver-dominant metastases from other primary malignancies.
Radiofrequency Ablation (RFA)
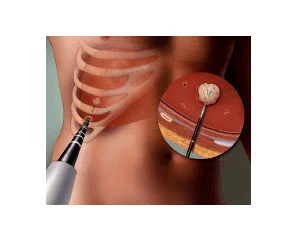
Radiofrequency ablation for cancer is a minimally invasive procedure that uses electrical energy and heat to destroy cancer cells.
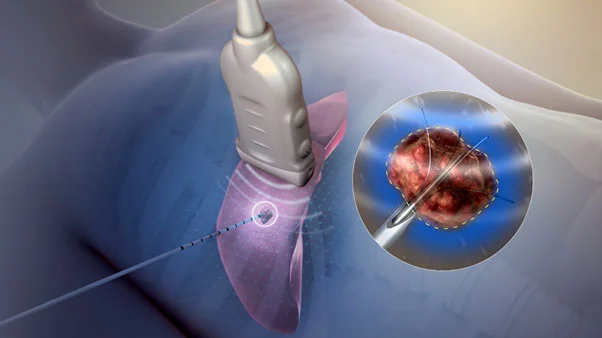
The radiologist uses imaging tests to guide a thin needle through the skin or through an incision and into the cancer tissue. High-frequency energy passes through the needle and causes the surrounding tissue to heat up, killing the nearby cells.
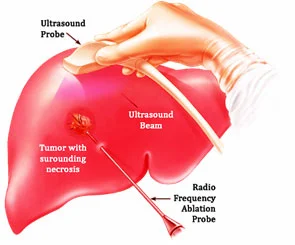
Radiofrequency ablation is most commonly used to treat a spot of cancer that is causing problems such as pain or other discomfort, and is generally not used as the primary treatment for most cancers.
Radiofrequency ablation is sometimes used to treat cancers in the:
- Adrenal gland
- Breast
- Bone
- Kidney
- Liver
- Lung
- Pancreas
- Thyroid
- Radiofrequency ablation is typically considered a treatment option only if you’re not a good candidate for surgery for some reason — such as your overall health or the presence of many small tumors in an organ.
- Radiofrequency ablation is one of several types of ablation therapy used to treat a wide range of conditions.
Book Appointment
-
Varicose Veins & Varicose Ulcer Treatment
-
Non-Healing Wound Management
-
Vascular Malformations
-
Uterine Fibroid or Prostate Embolization
-
Cancer Treatments – TACE, RFA, Embolization
-
Dialysis Access Catherization
-
Diagnostic Procedures – FNAC, Biopsy, Diagnostic Angiography
-
Abscess Treatment - Aspiration, Pigtail Drainage
-
Treatment of Aneurysm and Stroke
-
Deep vein thrombosis (DVT)
-
Other USG, CT & DSA Guided Interventions
